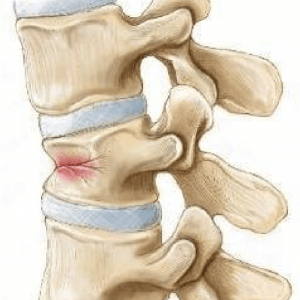
Osteoporotic Spinal Fracture
Osteoporosis Spine Fracture Treatment
Spinal Diseases
Back pain
Neck Pain
Slip Disc
Spinal Stenosis
Spondylosis
Spondylolisthesis
Cervical Myelopathy
Spine Fracture
Spine Tuberculosis
Spinal Tumors
Scoliosis
Kyphosis
Osteoporosis is a bone disease in which basic framework of bone is weakened. There is associated lack of calcium in the bone. This leads to fragile bones which are prone to fractures. Osteoporosis primarily affect old patients; however, in certain disease process it can affect young individuals also. These patients can then develop osteoporotic spinal fracture, which primarily affect thoracic spine; however, these fractures can happen in lumbar spine and cervical spine also.

Symptoms of Osteoporotic Spine Fracture:
Primary symptoms of osteoporotic spine fractures is pain at the site of fracture. Pain is more on weight bearing (sitting, standing, walking) and gets better with rest. There can be localized spine deformity at the site of fracture due to bone collapse. If part of fractured vertebra projects significantly in spinal canal, it can compress on spinal cord and can lead to symptoms of spinal stenosis (radiculopathy, tingling-numbness, loss of sensation and weakness in legs, loss of bladder-bowel control).
Diagnosis of Osteoporotic Spine Fracture:
Osteoporotic spine fractures usually present with history of fall with new onset/ increased back pain. Sometimes there is no history of trauma and vertebral fractures occur with routine day to day activities. This happens as weak bones are not able to withstand body weight. There may be associated with spinal cord compression symptoms.
- X-ray: As x-ray is cheap and easily available, it is usually done as first line of investigation. Also, x-ray is required to detect vertebral fractures. An osteoporotic spine will also show lack of calcium on x-ray.
- MRI Scan: If patient presents with symptoms of nerve compression, or if a surgical intervention is planned, an MRI will reveal amount of spinal stenosis, affection of other vertebrae, and other underlying disease.
- DEXA Scan: DEXA (Dual Energy X-ray Absorptiometry) is gold standard test to detect osteoporosis. A DEXA scan is useful as it will quantify osteoporosis , which will help in
- Classifying the grade of osteoporosis,
- Predicting risk of developing fracture,
- Assessing the need of treatment,
- Assessing response to treatment.
- CT Scan: A CT scan might be necessary in cases where MRI is contraindicated (patients with pacemaker, ear implants, stainless steel orthopedic implants). Newer CT based tools are also available to detect osteoporosis.
- Other tests to detect an underlying/ associated disease.
Treatment of Osteoporotic Spine Fracture:
The aim of treating osteoporotic spine fractures is two folds, 1) treatment of vertebral fracture, 2) treatment of osteoporosis as it is a generalized disease and affects all bones. A vertebral fracture usually heals in position with adequate bed rest (3-6 weeks), bracing, pain medicines and calcium-vitamin D supplements. Gradual rehabilitation with step-wise weaning off of brace is required over a period of 6-12 weeks. Repeated x-rays are done at regular intervals to assess bone healing and to rule out further vertebral collapse. Majority of the patients with osteoporotic vertebral fractures respond to this medical line of treatment. However, a subset of patients need surgical intervention. Following options are available:
- Kyphoplasty/ Vertebroplasty: If there is progressive vertebral body collapse on serial x-rays or persistent pain on follow up, a bone cementing procedure is recommended. A needle is inserted in the collapsed vertebra and liquid bone cement is injected. This cement then solidifies within vertebra and provides internal support. This causes immediate pain relief and prevents further vertebral collapse.
- Spine Decompression and Instrumentation Surgery: A spine fusion surgery is required
- If there is associated spinal stenosis from collapsed vertebra which requires spine decompression,
- If vertebral collapse is severe that there is no space for the cement to occupy.
- If vertebral fracture is causing spine instability.
In certain cases, a simultaneous vertebroplasty/ kyphoplasty procedure is done or the broken vertebra is reconstructed with metallic cage. One of the major limitation of spine instrumentation is poor hold of metallic implants in osteoporotic vertebrae. Various specialized spine instruments are used to get good hold in weak bone (cemented pedicle screws, HA coated pedicle screws, wires and cables).
It is very essential to simultaneously treat generalized osteoporosis also with medical treatment to strengthen other bones and prevent repeated fractures. Various medicines to strengthen bone (calcium, vitamin D), prevent calcium washout from the bone (calcitonin nasal spray, bisphosphonates) and improve basic framework of bone (Denosumab, Teriparatide) are used in different combinations as per the need of individual patient.
If you or a loved one is dealing with an osteoporotic spine fracture in Mumbai, don’t hesitate to reach out to Dr. Amit Sharma for expert care and answers to all your questions at +91-9967600461
What is an osteoporotic spine fracture?
An osteoporotic spine fracture occurs when a weakened vertebra in the spine collapses or fractures due to the loss of bone density and strength associated with osteoporosis.
How common are osteoporotic spine fractures in Mumbai?
Osteoporotic spine fractures are relatively common, especially among the elderly population in Mumbai. The prevalence of osteoporosis in India makes these fractures a significant health concern.
What are the symptoms of an osteoporotic spine fracture?
Common symptoms include severe back pain, reduced height, stooped posture, and potential nerve compression symptoms like numbness or weakness in the limbs.
How is an osteoporotic spine fracture diagnosed?
Diagnosis involves a thorough physical examination, imaging studies such as X-rays or MRIs, and bone density tests to assess osteoporosis severity.
What treatment options are available for osteoporotic spine fractures in Mumbai?
There are several treatment options, including:
- Conservative Management: Rest, pain management, and physical therapy.
- Kyphoplasty or Vertebroplasty: Minimally invasive procedures to stabilize and relieve pain.
- Medications: To address osteoporosis and prevent future fractures.
- Surgical Intervention: In severe cases, surgery may be necessary to restore vertebral height and stability.
What is Kyphoplasty, and how does it work?
Kyphoplasty is a minimally invasive procedure where a balloon is used to create space in the collapsed vertebra, followed by the injection of bone cement. This stabilizes the vertebra and alleviates pain.
What should I expect during the recovery process after osteoporotic spine fracture treatment?
Recovery varies depending on the treatment method but generally involves pain management, gradual return to activities, and, in some cases, physical therapy to improve strength and mobility.
Is osteoporosis treatment essential after an osteoporotic spine fracture?
Yes, addressing osteoporosis is crucial to prevent future fractures. Medications and lifestyle changes may be recommended to improve bone density and reduce the risk of recurrence.
How do I find the best specialist for osteoporotic spine fracture treatment in Mumbai?
Look for a spine specialist like Dr. Amit Sharma, known for expertise in treating osteoporotic spine fractures. Consider factors such as experience, patient reviews, and hospital affiliations.
Is surgery always necessary for osteoporotic spine fractures?
Surgery is not always required. Many cases can be managed conservatively or with minimally invasive procedures like Kyphoplasty. The treatment approach depends on the severity and specific circumstances of the fracture.
How can I prevent osteoporotic spine fractures in the future?
Preventive measures include a balanced diet rich in calcium and vitamin D, regular weight-bearing exercise, lifestyle modifications, and appropriate osteoporosis medications as recommended by your specialist.

A comprehensive breakdown on the intricacies of osteoporotic spine fractures – from symptoms to diagnostic measures, and from non-invasive treatments to surgical interventions. The emphasis on simultaneous treatment of the fracture and the underlying osteoporosis condition is particularly vital. For readers keen to delve into the broader spectrum of rehabilitation and the role of patient education, my article titled “Comparing Chiropractic and Physiotherapy Protocols with a Focus on Patient Education for Empowered Rehabilitation” provides an insightful perspective. As we navigate the complexities of spine health, it’s imperative to be equipped with knowledge and the right therapeutic approach.
Thank you.